Soybeans, with their heads held high.
Osteoporosis is a pathology with an increasing presence in society, driven by the increase in the average height of the population in recent decades and the increasing life expectancy. Based on clinical data recorded by the World Health Organization (WHO), 500 million people could currently suffer from the disease worldwide, and of them almost 3 million in Spain alone, with an associated health expenditure of more than 4,000 million euros, according to the Spanish Society of General and Family Physicians.
But beyond the numbers, osteoporosis is a serious health problem that affects the quality of life of those who suffer from it. A healthy, dense and well-mineralized skeleton supports the weight of the body, protects organs from impact damage and provides autonomy of movement. A porous skeleton, with low mineral content, becomes fragile and brittle over time. Fractures of long bones appear, such as the femur in the hip, or those that support more complicated structures such as the spine. Muscles are overloaded, nerves are compressed, joints become inflamed, the body becomes deformed. All of this happens slowly, sometimes over years, before the first symptoms appear.
To understand what is behind this process, why it affects older people more, especially women beyond menopause, and above all what role soy plays in all this, we must first talk a little about how it is developed and maintained. the human skeleton.

Human bones are essentially composed of two different and complementary parts: an organic cartilaginous matrix, mainly fibers of the protein collagen and other accessories, which grows during childhood and adolescence until reaching the height dictated by our genetics and our diet, and a rigid mineral matrix, calcium phosphate crystals with magnesium inclusions, which are deposited on it and confer structural resistance and load capacity.
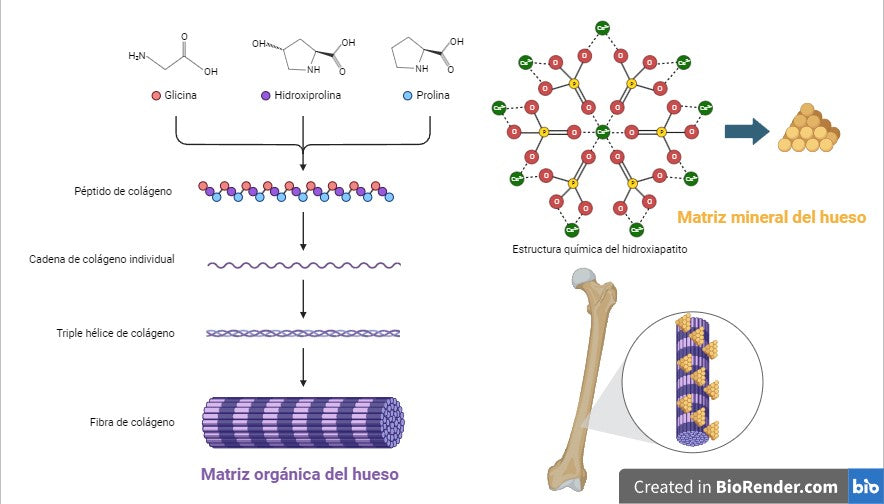
Each aspect of this structure is regulated by numerous environmental, hormonal and nutritional factors, but the engineers responsible for maintaining it are mainly two cell types integrated into the bone: osteoblasts and osteoclasts. Osteoblasts synthesize most of the components of bone, including collagen and hydroxyapatite, the crystalline form of calcium phosphate in the mineral matrix, and promote the growth and mineralization of cartilage (osteogenesis). Osteoclasts digest and reabsorb the mineral, reducing bone density and releasing calcium and phosphorus from the enormous reserves accumulated in the mineral matrix when the body needs it (bone resorption). The balance in the functioning of both types is known as bone remodeling, and properly regulated and nourished keeps the skeleton in perfect condition. However, when the balance is lost and bone resorption becomes dominant, the bone begins to lose mineral density, hardness and strength.
That is, osteoporosis begins.
Why is this balance lost in bone remodeling? On the one hand, the activity of osteoblasts and osteoclasts is highly controlled by the body through hormones such as testosterone and estrogen. During puberty, increased testosterone production in boys causes osteoblasts to speed up and osteoclasts to slow down, so their bones grow longer and denser, on average, than those of women of the same age and weight.
Estrogens help modulate balance, and during adulthood they contribute to maintaining skeletal health. Unfortunately, menopause causes a drastic decrease in estrogen production, and bone resorption becomes dominant. Postmenopausal women and other groups with estrogen deficiency are the main risk group for osteoporosis, without a single therapeutic approach that covers all cases. Some hormone replacement treatments that attempt to mimic the effects of estrogen in patients, such as SERM-type estrogen modulators, estrogen agonists such as raloxifene, or newer medications that seek to specifically affect bone components, such as romosozumab, They have been shown to have a beneficial effect against osteoporosis, but they usually present moderate to severe side effects, because estrogens are molecules with a large number of physiological functions and with receptors in many types of tissues in the body.
Another issue to take into account is that the skeleton acts as a natural reserve for many minerals, with calcium, phosphorus and magnesium as the main depositaries. Therefore, there is a continuous exchange of ions with the body that largely depends on the diet. A diet low in any of these three essential minerals will cause hyperactivation of osteoclasts to make them available to the rest of the body, and a balanced diet rich in them, although generally beneficial for the skeleton, may not help or be sufficient on its own if In addition, other molecules that are important for its correct metabolism are not ingested, such as vitamins D3 and K2, crucial for the absorption of calcium by the intestine and its fixation in the bones, or the amino acid glycine, a fundamental component of collagen and one of the molecules most in demand in the body, almost always in nutritional deficit. Nutritional supplementation can help improve these processes, but in cases like magnesium, not all formulations are equally effective. In short, you can't build a house without bricks.
And at this point we have to talk about soy, or more precisely about soy isoflavones. Isoflavones are phytoestrogens, plant compounds whose chemical structure is so similar to estrogens that they actually bind to their receptors and have physiological effects through them. Some, such as genistein or daidzein, have been shown to have diverse therapeutic potential for coagulation disorders, hypercholesterolemia and some types of cancer, and, of course, as estrogen replacement therapy in menopause and osteoporosis. Unfortunately, they carry penance in their sin, and often have some of the same side effects as medications like raloxifene.
In the late 1970s, research began on the possibility of developing modifications of soy isoflavones that would have the same beneficial properties with few or no side effects. The result was ipriflavone, a dadzein derivative that does just that.
Ipriflavone is a semisynthetic isoflavone; It does not exist naturally in soy and the body cannot synthesize it on its own, so it must be consumed as a supplement. Like its natural precursors, it can bind to estrogen receptors, but, and this is important, it does so with much greater affinity for the type β estrogen receptor (ER-β), the most abundant in bone, which makes to focus your activity there. Furthermore, although it binds to the receptor, it does not have estrogenic activity, and in fact it seems to favor the activity of the most common estrogen substitutes in replacement therapies by inducing an increase in the expression of that same ER-β.
In vitro studies have shown that the binding of ipriflavone to ER-β contributes to slowing down the functional maturation of osteoclasts, and therefore decreases bone resorption. At the same time, it promotes osteogenesis by facilitating the action of vitamin D on osteoblasts in two ways: 1) stimulating the synthesis of the active metabolite 25-hydroxyvitamin D, and 2) increasing the expression of the cellular receptor for the vitamin. This increases the absorption of calcium that becomes available to the bone.
At a clinical level, its action translates into an improvement in bone quality. Clinical studies show that the administration of ipriflavone in doses of 300 to 600 milligrams per day improves bone mineral density, increases blood calcium levels and decreases the levels of resorption markers in women with menopause and osteoporosis, contributing to a reduction of some typical symptoms of menopause such as hot flashes and bone pain, and a general improvement in the patient's quality of life. So that we can all walk with our heads held high.

Osteo Advance® with Ipriflavone is a food supplement designed to improve bone health, without gluten or genetically modified organisms. Contains:
• A combination of amino acids, vitamins and minerals that prevent bone loss and bone fragility fractures.
• Ipriflavone, a dual-action isoflavone without estrogenic activity, which promotes osteogenesis and inhibits bone resorption.
• Pure astaxanthin, a natural antioxidant that improves bone mineralization
Figures:
1. Figure 1: Common symptoms of osteoporosis and osteopathology
2. Figure 2: representation of the organic matrix and the mineral matrix of bone.
Collagen peptides, rich in glycine, hydroxyproline and proline, associate in an increasingly complex way in chains, triple helices and collagen fibers, which create the organic framework of the bone. Hydroxyapatite crystals, containing calcium phosphate, are deposited on collagen, giving the bone its hardness. Ca2+: calcium; O: oxygen; Q: phosphorus.
3. Action of ipriflavone on bone remodeling.
Ipriflavone is absorbed by the small intestine and binds to β-type estrogen receptors in bone. In osteoblasts, it facilitates the conversion of vitamin D into 1,25(OH)2D, its active form, and increases the expression of its receptor. Furthermore, it increases the expression of ER-β and promotes the release of the protein osteoprotegerin, which slows down the functional maturation of osteoclasts and decreases bone resorption. Ipr: ipriflavone; ER-β: estrogen receptor type β; OPG: osteoprotegerin; Vit D: vitamin D.
References:
(Hooshiar et al, 2022)
(Park and Weaver, 2012)
(Hu et al, 2020)
(Zhang et al, 2010; Vitale el at, 2018).



